
Credit: David Parkins.
Throughout 2021 and 2022, researchers at Ghent University Hospital in Belgium watched with cautious optimism as nearly 50 people with early stage Parkinson’s disease visited the clinic as part of a trial of a potential treatment1.
Everyday tasks had become difficult for these participants, who had been experiencing tremors, stiffness and difficulty walking. But over time, some of them seemed to be returning for follow-up appointments with a new lease of life.
“They were quicker, they were less stiff,” says study co-leader Patrick Santens, a neurologist at the University of Ghent. “They were having less trouble in their daily functioning, like eating, like putting on their clothes.”
Nature Outlook: The human microbiome
At the end of the trial, the researchers checked which of the volunteers had received the treatment and which had instead been given a placebo. For the half who received the treatment, the scientists found that participants’ scores on a widely used test of motor function had improved by an average of almost six points — a result that exceeded expectations, Santens says. Trials of treatments for Parkinson’s disease often show improvements of two or three points on the movement scale, but that doesn’t make a meaningful difference in people’s lives, he explains. Six points is clinically significant. “It’s quite something when you can achieve that.”
The nature of the treatment being tested was also a little surprising. It was not a high-tech designer drug with a price tag to match, or a complex regimen of pills, but rather a one-time delivery of gut microorganisms from healthy donors, bound up in faecal matter, into the digestive tract of people with Parkinson’s disease. Although faecal microbiota transplantation (FMT) has become widely accepted for the treatment of recurrent gut infections of harmful bacteria, its use for what is typically thought of as a brain condition is more unexpected.
More research will be necessary to confirm the results and clarify who is most likely to benefit from the procedure and which microbes are most crucial to the treatment’s success. This knowledge could contribute to efforts already under way to develop small-molecule drugs that target pathways linking the disease to the gut. But even as opportunities for treatment begin to be revealed, scientists still don’t have a clear picture of how — or even whether — the gut microbiome actually contributes to Parkinson’s pathology.
Microbial connections
Parkinson’s disease affects nearly 3% of people over the age of 65 globally. Its characteristic movement difficulties stem from a loss of neurons in a part of the brain called the substantia nigra pars compacta, which organizes fine motor skills. These neurons typically release the signalling molecule dopamine, and current treatments such as levodopa aim to alleviate Parkinson’s symptoms by replacing lost dopamine in the brain.
Yet the disease is not confined to the brain; a link to the gut has long been known. Most people with Parkinson’s, for example, experience constipation and trouble with food moving from the stomach to the small intestine. One-quarter of people with Parkinson’s also have a condition called small-intestine bacterial overgrowth, in which more bacteria than usual build-up inside the gut, causing symptoms including abdominal pain, weight loss and malnutrition.
Several studies have looked for evidence of changes in the composition of the gut microbiome. In the largest such study so far, published in 2022, researchers gathered stool samples from 490 individuals with Parkinson’s disease and 234 healthy controls and sequenced the DNA of the microbes present2.
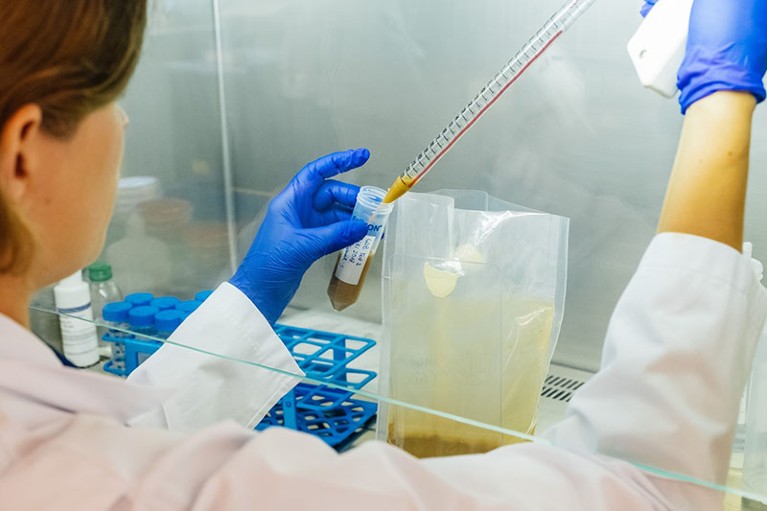
Researchers at Ghent University Hospital in Belgium prepare fluid for faecal transplantation in a trial to treat Parkinson’s disease.
The analysis revealed that, as a group, people with Parkinson’s disease experience widespread changes to their gut microbiota. “There are actually clusters — not individual microbes, but clusters of microbes — that tend to grow together or be depleted together,” explains Haydeh Payami, a geneticist at the University of Alabama at Birmingham, who led the study. Among the clusters are high levels of opportunistic pathogens, microbes such as Escherichia coli and Klebsiella that do not typically cause harm but can do so when the microbiota as a whole is out of balance. Species that digest dietary fibre and produce short-chain fatty acids — molecules that are known to be beneficial across many body systems — are severely depleted.
“There’s a lot of things that are going on,” says Payami. But the significant question that this leaves open is the relationship between the gut symptoms and the motor symptoms of Parkinson’s disease. “I do not know if the gut microbiome has anything to do with the pathology of Parkinson’s disease. Or is the gut getting sick because the person is sick with Parkinson’s?” she asks.
Abdominal beginnings
In 2003, researchers led by neuroanatomist Heiko Braak proposed that Parkinson’s disease might be caused by an unknown pathogen that enters the body through the gastrointestinal tract and travels to the brain along the vagus nerve — the neural highway linking parts of the digestive tract to the central nervous system3. Their paper crystallized interest in the idea of a gut origin for Parkinson’s: after all, it had long been known that some people have gut troubles years before developing the movement problems that trigger a Parkinson’s diagnosis.
More epidemiological evidence has since emerged to support Braak’s hypothesis. The presence of constipation or laxatives in a person’s medical history puts them at greater risk of developing Parkinson’s disease up to decades later4. By contrast, people who have their appendix removed seem to have a lower risk of developing the disease5. A procedure to sever the vagus nerve, which was once a common treatment for chronic heartburn, also reduces the risk.
Researchers have also found clumps of a protein called α-synuclein, a hallmark of Parkinson’s pathology, in gut neurons before the development of the disease. (Cells in the appendix express especially high levels of α-synuclein, which might explain why an appendectomy lowers risk.) Neurons in the gut make dopamine, and oxidized dopamine — which can be produced by gut inflammation — triggers α-synuclein clumping. Gut microbes themselves can produce molecules with a structure similar to α-synuclein. These α-synuclein ‘mimics’ can also form clumps, and might trigger clumping of α-synuclein itself.
“All of these molecules that are potentially involved in Parkinson’s disease are present in the gut,” says Elizabeth Bess, an organic chemist at the University of California, Irvine, who has investigated how chemical reactions performed by gut bacteria trigger α-synuclein clumping6.

Clumps of the protein α-synuclein, a hallmark of Parkinson’s pathology, have been found in gut neurons.Credit: BIOLUTION GMBH / Science Photo Library
The best evidence for a causal link between the microbiota and Parkinson’s comes from mouse studies. For example, mice genetically engineered to express excess α-synuclein will develop motor impairments similar to Parkinson’s disease. However, if they are raised in a sterile environment, preventing their guts from being colonized by microbes, these symptoms develop later than in mice with a typical complement of gut microbes7. Moreover, if gut microbes from people with Parkinson’s are transplanted into uncolonized mice, the mice develop more pronounced movement problems than do those that receive microbes from healthy donors. Mouse studies also suggest that α-synuclein clumping can move from gut to brain along the vagus nerve, although it is not clear whether the individual clumps that form in the gut are transported to the brain directly or trigger neighbouring molecules to form clumps in a self-propagating process8.
These and similar findings suggest that “some component of the microbiome potentially is pathogenic”, says Timothy Sampson, a microbiologist at Emory University in Atlanta, Georgia, who has contributed to mouse studies on α-synuclein. Other research suggests that the gut microbiota might contain factors that protect healthy people against Parkinson’s-related pathology — some gut bacteria, for example, can digest α-synuclein clumps9. However, the microbiota might hamper the effectiveness of Parkinson’s disease treatment: some bacteria are able to convert the drug levodopa into dopamine in the gut, whereas others break down dopamine itself, potentially reducing the dose delivered to the brain.
Therapeutic transplants
Suggestive though such findings might be, most researchers think that current evidence is not sufficient to say definitively whether alterations in the gut microbiome drive Parkinson’s disease in humans. Many suspect that there are multiple aetiologies, with some people experiencing ‘gut-first’ disease, and others ‘brain-first’ disease10. One reason why it is so difficult to untangle the causal relationships is that gut symptoms are fairly non-specific, says Laurie Sanders, a neuroscientist at Duke University in Durham, North Carolina. “There are lots of reasons why somebody might have gut dysbiosis and changes in their microbiome” she says. Until we have a way to intervene to see if that’s going to reduce incidence of Parkinson’s up front, she adds, it’s going to be hard to answer questions of cause and effect.
Mouse studies again provide some hope that altering the gut microbiota could indeed alter the course of Parkinson’s pathology. In mice with Parkinson’s symptoms caused by exposure to the pesticide rotenone, FMT from healthy mice restores the normal gut-microbial community and improves movement symptoms11. In another mouse model of neurotoxicant-induced Parkinson’s disease, FMT from healthy human donors also reversed neurodegeneration and motor symptoms12.
Researchers have now begun early-phase clinical trials of potential Parkinson’s treatments that target the gut13. One possibility is dietary fibre supplementation to promote the growth of fibre-fermenting bacteria. This intervention has been shown to increase bacterial production of beneficial short-chain fatty acids in people with Parkinson’s, but so far only to levels that are still lower than those in healthy controls14.

Geneticist Haydeh Payami at the University of Alabama at Birmingham found that people with Parkinson’s disease experience widespread changes to their gut microbiota.Credit: University of Alabama at Birmingham
FMT studies have also yielded some puzzling surprises. In Santens’s double-blind trial, for instance, researchers found that people in the placebo group, who received an infusion of their own gut microbiota, improved by an average of 2.7 points on the movement scale. Some other FMT trials have also suggested a placebo effect.
As a next step, Santens is using the data from his trial to inform the design of a larger one that he and a group of colleagues aim to launch by early 2026. First, he is looking for bacterial species or other donor characteristics that correlate with treatment success. So far, there is no clear component or source of faecal material that seems necessary for success. “There is no real ‘super donor’ effect,” he says. There are, however, signs that people with severe constipation benefit less from the transplant, and would therefore not be the ideal target population.
Payami is also digging deeper into the data from her analysis of Parkinson’s microbiota with an eye towards individualized therapy. In a preprint posted on medRxiv, which has not yet been peer reviewed, she and a team including Sampson have begun to characterize subgroups of people with the disease according to the specific ways that their gut microbiota differ from ones typically found in people without the disease15. One subgroup, for example, includes people who harbour elevated levels of opportunistic pathogens, whereas individuals in another lack fibre-fermenting bacteria. About 20% of the group do not have a disrupted microbiota at all. The analysis points the way towards using microbiota characteristics as a biomarker to guide treatment, she says.
Harnessing mechanisms
But treatments that aim to broadly alter the microbiota might not be the ultimate goal. Some scientists are investigating the mechanisms underpinning the gut microbiota’s contribution to Parkinson’s disease, with the aim of developing more targeted treatments.
“The microbiome is extremely malleable. For a long time, we’ve thought that that makes it a better target for inhibiting disease processes,” says Bess. But some scientists are questioning that view. “An emerging perspective is that because it’s so malleable, it’s hard to drug,” she says. Instead, modulating the body’s response to gut microbiota activities might prove simpler and more durable.
Bess’s team, for example, has identified one mechanism by which E. coli might contribute to Parkinson’s-related pathology in the gut. The bacterium’s growth, especially in the presence of gut inflammation, results in the oxidation of iron and then dopamine, which triggers the clumping of α-synuclein. The researchers have also identified a molecule called caffeic acid, which can interrupt this chain of events and inhibit the formation of α-synuclein aggregates, at least in laboratory dishes16.
Another team of researchers has zeroed in on a molecule produced by E. coli called curli — an α-synuclein mimic that, in mice, is also associated with Parkinson’s-like pathology in the brain17. The researchers also demonstrated that a molecule derived from green tea can dampen curli’s effect on α-synuclein aggregation, and prevent the protein from clumping. Axial Therapeutics, a biotechnology company in Woburn, Massachusetts, co-founded by study team member and microbiologist Sarkis Mazmanian at the California Institute of Technology in Pasadena, is now developing a drug based on this molecule.
Other researchers are working to fill in the bigger picture. So far, much of the research on microbiome changes in Parkinson’s disease consists of “snapshots”, Sanders says — there has been a paucity of long-term cohort studies focused on the gastrointestinal aspects of Parkinson’s disease. The result is a lack of knowledge about how the gut microbiome might shift as the disease progresses.
Sanders co-leads the Coordinating and Data Management Center for the Gut–Brain Communication in Parkinson’s Disease Consortium, an effort launched last year by the US National Institutes of Health (NIH) to gather detailed information on gut symptoms and microbiome alterations in people with Parkinson’s, and track those changes over time. The team is now developing protocols for recruitment of participants, says Sanders, and is “cautiously optimistic” about having its funding renewed for a second year, despite the disruptions to NIH research that have occurred during US President Donald Trump’s administration.
Payami is also continuing to track gut microbiome changes in individuals who have been part of previous studies in her lab — a total of 180 people with Parkinson’s and 130 healthy controls, with between 4 and 8 years of follow-up so far. Payami expects to complete analysis of microbial DNA sequences from these samples this summer.
Despite the unknowns, Payami is optimistic about the potential of gut-based therapies for Parkinson’s. Even if the pathology doesn’t begin in the gut, it almost always ends up there, and offering relief for these symptoms is worthwhile in itself. If therapies targeting the gut microbiota could slow disease progression too, she says, “that would be the cherry on top”.





